Pharmacy professionals share a common goal to ensure the safe and effective use of medications for their patients. Unfortunately, inadequate or absent prescriber communication is a persistent barrier to good care. According to a recent ISMP Canada report, medication incidents related to communication breakdowns accounted for eight per cent of harmful incidents reported in Manitoba.
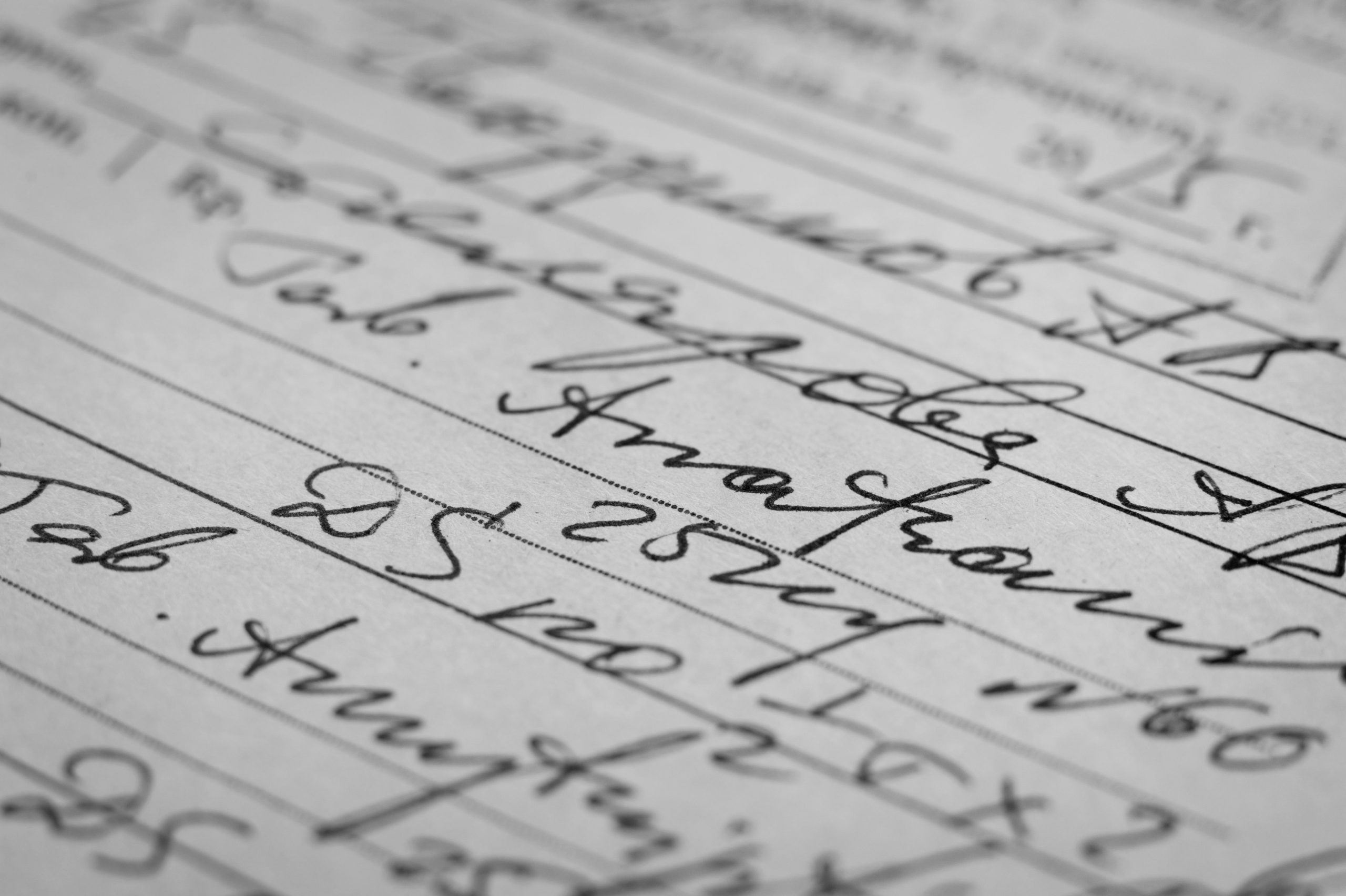
Prescription clarity and coordination between healthcare providers were identified as critical areas of focus in these incidents. Prescription clarity refers to the accuracy, completeness, and consistency of medication information provided by the prescriber. Ambiguous, conflicting, or incomplete information in the prescription can lead to misinterpretation of key medication information and ultimately harm to the patient.
Incident Examples from Manitoba Community Pharmacies
One example of a prescription clarity issue was when a pharmacy received a faxed prescription with instructions for diazepam 5 mg daily for one week and diazepam 2 x 2 mg daily for one week – with a note at the bottom of the page that said, “BENZO taper.” The pharmacist interpreted this to be 1 week of 5 mg daily and then 1 week of 4 mg daily. The prescriber intended this to be 9 mg daily (as a taper from the patient’s usual 10 mg daily). The patient took 2 x 5 mg daily to make up the dose, after which the error was discovered.
Another example involved a patient’s death due to a potentially unclear prescription. A physician contacted the pharmacy to request prescription records for a patient who had passed away. The death investigation suggested that benzodiazepines contributed to the patient’s death. The patient’s prescription vial label indicated 1 mg twice daily, while the physician intended a dose reduction to 0.5 mg twice daily. The legibility of the dose change on the prescription could not be determined due to damaged pharmacy records.
Clear, Standardized Communication is Key to Preventing Medication Incidents
To promote adequate communication, pharmacy professionals must work closely with prescribers to develop a clear and consistent communication plan. Pharmacy teams should develop a template for communicating with prescribers about prescription clarifications like dose and frequency. This template should clearly document how the prescription has been interpreted to facilitate necessary corrections.
Your team should also consider standardized forms of communication to support prescription handoff within your pharmacy.
It is also essential to maintain accurate records of all communication with the prescriber, including verbal and written instructions.
Medication incidents resulting from communication breakdowns between prescribers and pharmacists are preventable. Prescription clarity and coordination between healthcare providers are critical in ensuring the safe and effective use of medications for your patients. Pharmacy professionals must continue to work collaboratively with prescribers on improving communication to ensure optimal patient outcomes.