1. What is an Independent Double Check?
Pharmacy professionals use independent double checks to detect and prevent potential medication incidents. Two people must complete the double check without knowledge of one another’s results. If a pharmacy technician prepares a medication, for example, then a pharmacist could check for accuracy.1
To be clear, an independent double check is not a review of another person’s work. Instead, two people perform separate checks that they compare once they are complete.
Healthcare professionals are better at noticing another person’s mistake. This means that two people working apart reduces the chance of an error.
When there is only one person available in the pharmacy, they can’t do a double check. In this case, the professional can conduct a delayed self-check hours or days after the first check.2
2. Why do We Need to Complete Independent Double Checks?
Independent double checks are a way to lessen confirmation bias. Confirmation bias is a cognitive bias common to most people. Confirmation bias means that are more likely to perceive what we expect. We are also less likely to perceive information that contradicts our expectations.
Because we already have a set expectation, we are less likely to detect a mistake. For example, if a person chooses the wrong drug, they are unlikely to see their mistake. They will see the correct drug because that is what they expect to see. Having another person perform the same check will boost the chance of accuracy.4
You can further reduce confirmation by
- teaching pharmacy staff about confirmation bias;
- segregating look- and sound-alike drugs;
- checking patient profiles and medical history to identify potential medication incidents; and
- asking patients open-ended questions about their understanding of their medications.3
3. Are Independent Double Checks Effective?
Independent double checks can detect up to 95 per cent of near-miss events.2
One study observed pharmacist independent double checks on 1,645 anti-cancer parenteral orders. During these checks, pharmacists detected 30 errors in the first check and 10 errors in the second.5
This means that a second independent check increased error detection by 33.3 per cent.
4. When is the Best Time to Conduct an Independent Double Check?
There are times when pharmacy professionals can’t conduct independent double checks. High workloads and time constraints put pressure on pharmacy teams. It is important that you are selective about independent double checks.
You can limit your pharmacy’s double checks to the most impactful and risky processes:
- High-alert medications that can cause serious harm to a patient. Examples include direct oral anticoagulants and direct thrombin inhibitors;
- High-risk processes such as compliance packaging, opioid agonist therapy, or compounding; and
- High-risk patient populations such as older adults and pediatric populations.2,4
Fewer, more focused independent double checks are the most effective verifications.2
You might be tempted to skip independent double checks during demanding periods. When our workload is high or stressful, our confirmation bias worsens. It is especially critical that you conduct independent double-checks during high-stress situations.6
5. How Do We Apply Effective Independent Double-Checks in Practice?
Your pharmacy should have a standardized process for independent double-checks. This will help prevent inconsistencies among different people performing the checks. The pharmacy manager should train pharmacy staff on the verification process.
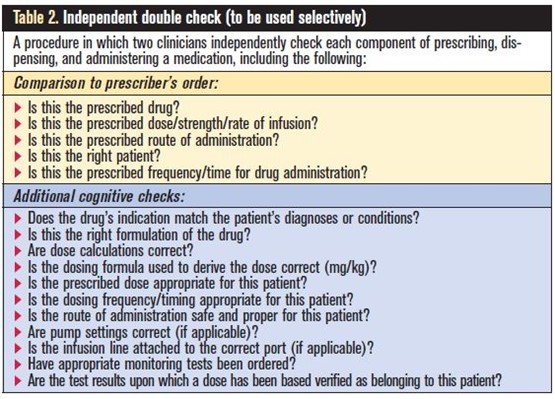
You can create a checklist to remind pharmacy professionals of the essential steps:2
Confirmation bias is a tricky and common phenomenon in human cognition. Selective and well-structured independent double checks are a key tool to lessen confirmation bias and prevent medication incidents.
References:
- Billstein-Leber, M., Carrillo, C., Cassano, A. T., Moline, K., & Robertson, J. J. (2018). Guidelines on Preventing Medication Errors in Hospitals. American Society of Health-System Pharmacists. Retrieved August 8, 2022, from https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/preventing-medication-errors-hospitals.ashx
- Independent Double Checks: Worth the Effort if Used Judiciously and Properly. Institute For Safe Medication Practices (ISMP). (2019, June 6). Retrieved August 8, 2022, from https://www.ismp.org/resources/independent-double-checks-worth-effort-if-used-judiciously-and-properly
- Practice Insight: Avoiding confirmation bias. Pharmacy Connection. (2021). Retrieved August 8, 2022, from https://pharmacyconnection.ca/practice-insight-avoiding-confirmation-bias-winter-2021/
- Santa Checks His List Twice. Shouldn’t We? Institute For Safe Medication Practices (ISMP). (2009). Retrieved August 8, 2022, from https://www.ismp.org/resources/santa-checks-his-list-twice-shouldnt-we
- Booth, J. P., Kennerly-Shah, J. M., & Hartman, A. D. (2022). Description of the role of pharmacist independent double checks during cognitive order verification of outpatient parenteral anti-cancer therapy. Journal of oncology pharmacy practice: Official publication of the International Society of Oncology Pharmacy Practitioners, 28(2), 381–386. https://doi.org/10.1177/1078155221994319
- Lee, J. D., Wickens, C. D., Liu, Y., & Boyle, L. N. (2017). Designing for people: An introduction to human factors engineering. CreateSpace.



